Introduction
The literature suggests a widespread reduction in the availability and accessibility of newer treatment options among marginalized groups in AML. Studies from large national databases point to lower socio-economic status, Hispanic and African American race, Medicare or no insurance, being unmarried, treatment at non-academic centers, and rural residence as negatively impacting overall survival (OS) and rates of chemotherapy utilization in AML patients (Patel et al. 2015, Jaco et al. 2017, Bhatt et al. 2018, Master et al. 2016). We hypothesized that facility affiliation and pt volume would also have important effects on time to treatment (TTT) and OS in AML, even when these socioeconomic disparities were accounted for.
Methods
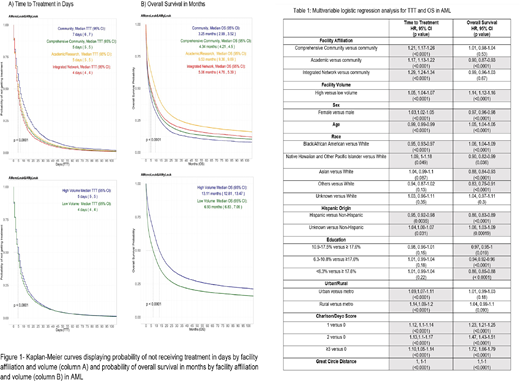
For this retrospective analysis, we used NCDB data that included 124,988 pts over the age of 18 with AML between the years 2004-2016. Variables analyzed included facility types described as community cancer programs (CP), comprehensive community cancer programs (CCP), academic/research center cancer programs (AC) and integrated network cancer programs (IN), and volume of facilities defined as high volume (HV) and low volume (LV). HV facilities had case volumes of ≥ 99th percentile and all other facilities were classified as LV. Multivariate analyses (MVA) included demographic and socioeconomic covariables. We used Cox proportional hazard analysis for both TTT and OS MVA. The Kaplan-Meier method was used to estimate median TTT and OS, and the log rank test used to compare TTT and OS across predictor variables.
Results
The median age of AML patients was 63 yrs (range 18-90) with 54% males, and 86% Caucasian. Five percent of patients were treated at CP, 30% at CCP, 44% at AC, and 10% at IN. 21% at HV facilities and 79% at LV facilities.
Median TTT in days at CP facilities was 7, compared to 5 days in CCP and AC facilities versus 4 days at IN (p<0.0001). TTT was 5 days at HV facilities versus 4 days at LV facilities (p<0.0001). Kaplan-Meier curves showed that TTT was similar between HV and LV facilities(figure 1). The median OS was 3.25 months in CP compared to 4.34 months at CCP, 5.06 months at IN and 9.53 months at AC (p<0.0001). For facility volume, the median OS was 13.11 months in HV facilities compared to 6.93 months in LV facilities (p<0.0001).
When sex, race, age, Hispanic Origin, education, urban/rural residence, Charlson-Deyo Comorbidity score and Great Circle Distance were adjusted for in MVA (table 1), the OS was higher in AC versus CP facilities (hazard ratio [HR] of 0.90 (0.87-0.93, p<0.0001), and there was no statistically significant difference with comparison of other facility types to CP. Similarly, there was a lower OS at LV versus HV facilities with a HR of 1.14 (1.12-1.16, p<0.0001). CCP facilities had a shorter TTT compared to CP with a HR of 1.21 (1.17-1.26, p<0.0001). AC had a shorter TTT than CP with a HR of 1.17 (1.13-1.22, p<0.0001), and IN had a shorter TTT compared to CP with a HR of 1.29 (1.24-1.34, p<0.0001). Additionally, TTT in the MVA for facility volume was shorter in LV facilities compared to HV facilities with HR of 1.05 (1.04-1.07, p<0.0001) [table 1].
Conclusion
When adjusting for various socioeconomic factors, we found that TTT was longest in CP compared to CCP, AC, and IN. Treatment at a LV facility resulted in a decreased overall survival. LV facilities may be less familiar with treatment regimens for AML, less likely to use novel treatment options, and be less familiar with the disease. We showed that treatment at an AC compared to CP, CCP and IN facilities improved survival. Given poor outcomes for AML, these results show the importance of going to AC and HV facilities with more experience in treating AML for improved outcomes.
Lai:Astellas: Speakers Bureau; Jazz: Speakers Bureau; Abbvie: Consultancy; Agios: Consultancy; Macrogenics: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal